Healthcare Fraud Detection Market: Global Outlook, Growth Drivers, and Competitive Landscape (2024–2030)
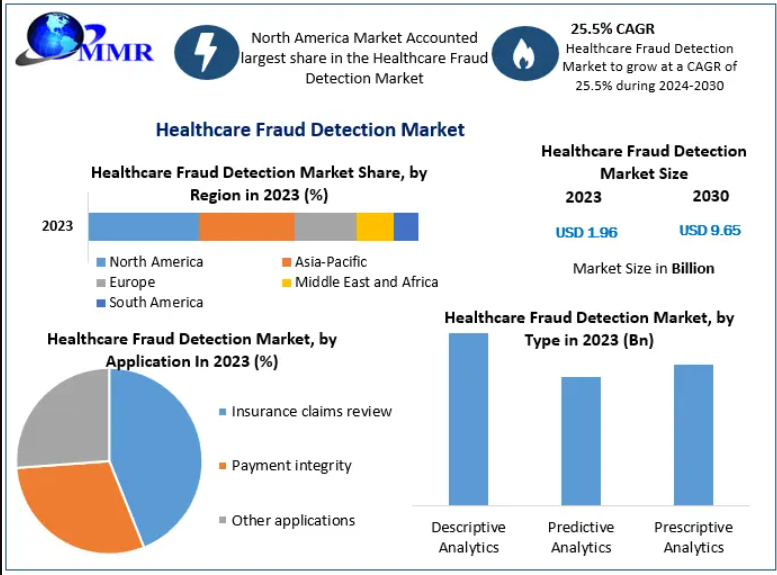
The Healthcare Fraud Detection Market is entering a phase of rapid acceleration as global healthcare systems face rising pressure to minimize fraud, waste, and abuse. Valued at USD 1.96 billion in 2023, the market is projected to surge to USD 9.65 billion by 2030, growing at an impressive CAGR of 25.5%. This growth reflects not only increasing fraud incidence but also the expanding role of analytics, automation, and AI-driven tools in modern healthcare operations.
Market Overview
Healthcare fraud—ranging from inflated claims and duplicate billing to phantom providers—continues to impose enormous financial strain on public and private healthcare payers worldwide. As digital health systems become more complex, detecting fraud proactively rather than reactively has become essential.
The industry has therefore seen a shift from traditional rule-based detection to more powerful predictive analytics, machine learning algorithms, and prescriptive tools capable of identifying patterns well before financial losses occur.
Post-pandemic digitalization further intensified the need for fraud detection technologies. COVID-19 introduced large-scale telehealth adoption and rapid claims processing, inadvertently widening the scope for fraudulent activities. This elevated the demand for robust fraud monitoring systems across regions.
To know the most attractive segments, click here for a free sample of the report:https://www.maximizemarketresearch.com/request-sample/3398/
Impact of COVID-19
The pandemic delivered a multifaceted impact:
- Short-term: Surge in fraudulent claims and misuse of emergency billing codes.
- Long-term: Permanent adoption of digital infrastructures that increased the need for sophisticated fraud monitoring tools.
- Regional variation: Different levels of lockdown severity across countries led to inconsistent fraud patterns, shaping a geographically varied demand curve.
This environment pushed healthcare stakeholders to adopt advanced fraud detection solutions sooner than expected, strengthening long-term market prospects.
Market Segmentation
- By Type
- Descriptive Analytics – Provides trend-based insights and retrospective analysis.
- Predictive Analytics – Forecasts potential fraud using statistical algorithms.
- Prescriptive Analytics – Suggests actionable strategies to prevent fraud, emerging as the fastest-growing segment.
- By Component
- Software (High-growth segment)
Growth is driven by:- AI-based risk scoring
- Real-time claim analytics
- Interoperability across payer systems
- Services – Consulting, integration, training, and managed services.
- By Delivery Mode
- On-premises (Largest Share)
- Preferred by organizations seeking strict data control
- Eliminates large upfront hardware investments
- Cloud-based Solutions
- Cost-effective, scalable, real-time monitoring
- Gaining traction as payers modernize IT infrastructures
- By Application
- Insurance Claims Review – The backbone of fraud detection, covering claim verification, anomaly tracking, and fraud scoring.
- Payment Integrity – Ensures accurate reimbursement and prevents improper payments.
- Other Applications – Provider authentication, eligibility checks, audit management.
- By End User
- Private Insurance Payers – Largest adopters due to high claim volume and financial exposure.
- Public/Government Agencies – Increasing investments driven by regulatory mandates.
- Employers – Growing awareness of insurance claims misuse.
- Third-party Service Providers – Outsourced analytics and fraud management partners.
To know the most attractive segments, click here for a free sample of the report:https://www.maximizemarketresearch.com/request-sample/3398/
Regional Analysis
North America
Dominates the global market due to:
- High healthcare expenditure
- Strong regulatory frameworks
- Rising fraud cases
- Significant investments in AI-driven healthcare IT
The U.S. remains the key revenue generator, supported by Medicare and Medicaid fraud control initiatives.
Europe
Steady growth driven by:
- Expansion of national healthcare digital systems
- Strict compliance requirements
- Increasing fraud investigation budgets
Countries like Germany, the UK, and France are leading adopters.
Asia-Pacific
Expected to witness the fastest growth, fuelled by:
- Rapid digitization of healthcare infrastructure
- Growing insurance coverage
- Rising medical tourism
- Government encouragement for analytics adoption
India, China, Japan, and Australia represent dynamic growth pockets.
Middle East & Africa
Gradual adoption with strong potential in Gulf countries as healthcare systems modernize and private insurance grows.
South America
Brazil and Argentina are investing heavily in digital health systems, creating opportunities for fraud prevention platforms.
Market Drivers
- Rising Healthcare Fraud Incidents
Billing scams, false claims, and identity misuse continue to escalate, pressuring payers to adopt automated fraud detection.
- Growth of Big Data and AI in Healthcare
AI and machine learning enhance accuracy, reduce manual review, and identify hidden fraud patterns.
- Expanding Healthcare Insurance Penetration
More insured individuals increase claim volumes, intensifying the need for fraud analytics.
- Government Initiatives
National policies to combat healthcare fraud (especially in the U.S., Europe, and APAC) are fueling adoption.
Market Restraints
- Reluctance in Developing Countries
Low awareness, limited budgets, and lack of trained professionals hinder adoption.
- Integration Challenges
Legacy healthcare systems often lack interoperability, complicating seamless implementation.
Competitive Landscape
The market is extremely competitive and innovation-driven. Leading companies focus on advanced analytics, cloud delivery, strategic partnerships, and AI-enhanced fraud management platforms.
Key Players
- LexisNexis (RELX Group)
- Pondera Solutions
- Northrop Grumman
- DXC Technology
- CGI Group
- HCL Technologies
- Conduent
- Wipro
- SCIO Health Analytics
- SAS Institute
- Fair Isaac (FICO)
- McKesson
- Verscend Technologies
- Optum (UnitedHealth Group)
- IBM
- Cotiviti, Inc.
- SCIOInspire Corp.
- Codoxo
- HMS
- EXL Service Holdings
- Change Healthcare
- Canadian Global Information Technology Group
Research Methodology (Summary)
The market assessment utilizes:
- Top-down and bottom-up market sizing
- Data triangulation techniques
- Insights from Bloomberg, Hoovers, Factiva
- Validation through expert interviews with technology providers, insurers, and industry consultants
This structured methodology ensures precise forecasting and a well-rounded market understanding.
Conclusion
The Healthcare Fraud Detection Market is poised for exceptional growth as fraud complexities rise and digital infrastructures expand globally. With AI-powered analytics, cloud-based platforms, and prescriptive strategies becoming mainstream, the industry is transitioning from reactive fraud management to a proactive, intelligence-led ecosystem.
Organizations that prioritize early adoption will not only reduce financial losses but also strengthen operational efficiency, compliance, and patient trust.